Is it necessary to perform a biopsy before MOHS surgery?

Is it necessary to perform a skin biopsy before MOHS surgery?
TB or not TB (to biopsy or not to biopsy)

Skin biopsies for histological examination are an old and important means used in dermatology for the advanced diagnosis of lesions whose clinical and/or dermoscopic appearance is not clearly diagnostic. In dermatology they are a part and continuation of the physical examination and not necessarily in the popular context that immediately links biopsy to cancer. As such, they are of great importance for assisting in diagnosis and, as a result, in therapeutic decisions regarding various skin problems, infectious, inflammatory, degenerative, and more.
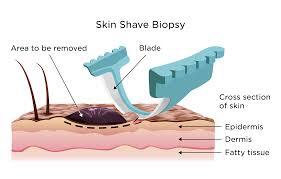
Skin biopsy using the shaving method
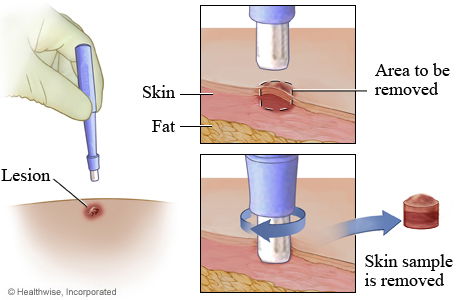
Skin biopsy using the punch method
Biopsies are also very important in dermatology in the diagnosis of cancerous skin lesions - originating from the skin cells themselves or tumors from other sources such as melanocytic, Merkel cells or metastases of tumors from other sources in the body.
At the same time, there are situations in which the importance and need for a diagnostic biopsy is less indicated and sometimes such biopsies may be unnecessary or even harmful. This is true mainly in keratinocytic skin tumors such as basal cell carcinoma also known BCC or squamous cell carcinoma and in its foreign abbreviation - SCC and especially in lesions located on the skin of the face, scalp and in cases ultimately intended for surgery using the Mohs method.
In over 90% of lesions suspected of keratinocytic malignancy in the skin of the face and scalp, a correct diagnosis can be reached based on a combination of clinical examination and dermoscopic examination - as proven in controlled studies published over the years. When the suspicious lesion is such that there is a potential to eventually be excised using the Mohs method, in which the pathological examination is performed during the surgery and in cases where it is necessary (for example when the histological finding in the surgery is not a definite finding) the tissue is also sent for a formal pathological examination with special dyes and markers.
Dermoscopic examination of a lesion on the subject's skin
So what are the disadvantages of a preliminary biopsy in this group of tumors, (in particular before excisional surgery using the Mohs method) and when is it better to avoid a biopsy?
From the patient's point of view, a biopsy is another procedure designed to diagnose the nature of the lesion. The wait for the appointment to perform the biopsy may be long, and even after the biopsy, in most cases, a long wait is expected until the pathological answer is received. After receiving a positive answer confirming the presence of a tumor, an appointment for further surgery must be arranged, an arrangement that often involves additional waiting and all the waiting may add up to significant periods of time. Beyond the immediate discomfort of performing the procedure and recovering from it, of the possible complications, the patient is exposed to a prolonged period of uncertainty, fear and perhaps even anxiety about what is happening in his body.
In terms of the lesion - in cases where the lesions are not large - often the biopsy may obscure the location of the lesion in such a way that it cannot be identified or located precisely (unfortunately, there is usually no accurate written or digital recording of the location of the biopsy). The period of time that passes between taking the sample and arriving to the final surgry often allows the skin to heal in a way that erases the evidence completely, so the exact location can’t be identified. The result may be a Mohs operation or a regular operation that does not involve the exact location of the tumor and yields a false negative answer. The tumor may appear after a while, near the surgical site... When the sampled lesion is larger and the biopsy removes only part of the lesion, a scar is formed inside the lesion that may hide tumor remnants within it on the one hand and on the other hand may damage the continuity of the tumor. When trying to follow the extensions of the tumor (in Mohs surgery) a false impression may be created as if we have reached uninvolved skin and the tumor has been removed in its entirety, while at a small distance from there, a tumor may continue to exist that will return later. (Such a situation, by the way, is common and often happens after an attempt to treat a cancerous lesions using liquid nitrogen). The operation of the biopsy itself may detach pieces of tumor and transport them along the path of the biopsy, thus seeding pieces of tumor in a location separate from the original tumor. Such an occurence (many have been documented and even published) may result in an excision surgery ending with the impression that the tumor has been removed in its entirety, even though a new tumor develops from the tissue seeded in the biopsy operation not far away.
Additional problems that may arise from a referral for a biopsy - not infrequently in the period of time that passes from the time of the examination by the referring doctor to the arrival at the doctor performing the biopsy (usually a plastic surgeon), the lesion changes and sometimes becomes less prominent and less obvious. In addition - the doctor performing the biopsy also has his own clinical considerations and in most cases he is not equipped with a dermatoscope which can help with identifying the exact location of the lesion intende to be biopsied. As a result, the biopsy can be performed from an inaccurate location and not sample the lesion/tissue for which the patient was referred for biopsy. Such a communication failure can cause a significant tumor to be missed, while both the referring doctor, the performing doctor and the patient are sure that everything is fine. The latter problem now has an available and recommended solution, which is marking and photographing the lesion on the patient's phone so that he can show the doctor performing the biopsy the exact location requested. In conclusion - in cases where we are dealing with lesions in which malignancy is suspected and there is a reasonable chance that an excision surgery using the MOHS method will be required - it is advisable to first perform a thorough dermoscopic examination to identify if there are any distinct signs of a tumor. If the finding is clear - there is no reason to perform a biopsy and it is possible and even desirable to refer the patient straight to a Mohs surgeon who will also perform a definitive resection. On the other hand, in cases where the nature of the lesion is not clear and it is not clear whether it is a malignant lesion - a good photo of the lesion should be taken on the patient's phone and sent with the photo to perform the biopsy. When referring for a biopsy, the patient should be instructed to ask the doctor performing the biopsy to document the location of the biopsy well in writing and with a photo so that if further surgery is required - the surgeon will be able to identify the location of the lesion sampled and operate in the exact right place.
It is important to remember that with all the importance of the biopsy as a first-rate diagnostic tool - the biopsy itself may have unwanted consequences and it is always advisable to consider the advantages and disadvantages of performing it.